Aorta Disease and Marfan Syndrome
The aorta is the large artery that leaves the heart and provides oxygen-rich blood to the rest of your body. These two things can cause the aorta to widen or tear. This raises the chance of things like:
- Atherosclerosis (hardening of the arteries)
- High blood pressure
- Genetic conditions such as Marfan syndrome and Turner syndrome
- Connective tissue disorders that affect the strength of the blood vessel walls, such as scleroderma, osteogenesis imperfecta, and polycystic kidney disease
- Injury
People with aorta disease should be treated by an experienced team of cardiovascular specialists and surgeons.
Arrhythmia
It may feel like your heart skipped a beat, added a beat, is “fluttering,” or is beating too fast (which doctors call tachycardia) or too slow (called bradycardia). Or, you might not notice anything, since some arrhythmias are “silent.”
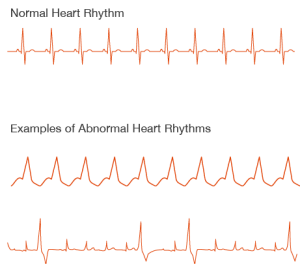
Causes and Types of of Arrhythmias
You could have an arrhythmia even if your heart is healthy. Or it could happen because you have:
- Heart disease
- The wrong balance of electrolytes (such as sodium or potassium) in your blood
- Changes in your heart muscle
- Injury from a heart attack
- Healing process after heart surgery
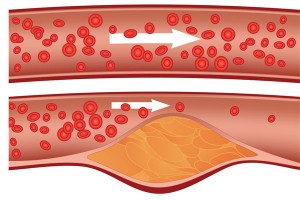
Atherosclerosis
Atherosclerosis is a process in which blood, fats such as cholesterol, and other substances build up on your artery walls. Eventually, deposits called plaques may form. The deposits may narrow or block your arteries. These plaques can also rupture, causing a blood clot.
It’s the condition that causes most heart attacks and strokes.
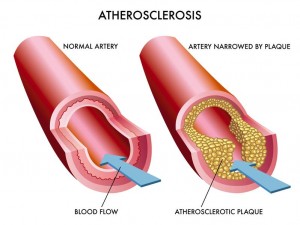
Over time, atherosclerosis can lead to:
- Angina – usually a pain or discomfort in your chest. This happens when your heart muscle isn’t getting enough blood.
- Heart attack – if the fatty material breaks down and a blood clot forms, it can completely block your artery and cut off the supply of blood to your heart. This is a heart attack.
- Stroke – when enough blood can’t get to your brain. If the blood supply is limited for a short time this can cause a mini-stroke (called a TIA). If the fatty material breaks down and a blood clot forms, it can completely block the artery.
- Peripheral arterial disease (or PAD) – when enough blood can’t get to your leg muscles. This can cause pain in your calves, hips, buttocks and thighs – usually when you’re walking or exercising
There are no visible symptoms of atherosclerosis until you suffer from angina or have a heart attack.
Regular health checks, especially if you are over 40, will check your risk of having a heart attack, and based on your results, your GP can tell you how to keep your heart healthy.
Angina
Angina is a feeling of chest pain or discomfort, typically during activity such as walking, or when you have strong emotions.
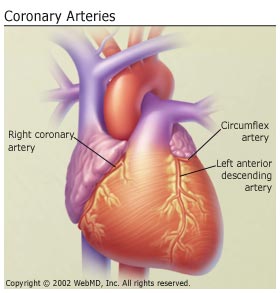
You may experience this if your heart is not getting enough blood and oxygen. This may be caused by a narrowing of the coronary arteries.
Each person may experience different sensations, so it is important that you know and recognise your symptoms:
- Dull pain, tightness or heaviness in the centre of your chest
- A squeezing or choking sensation
- Shortness of breath
- Pain in the shoulders and/or arms
- Sometimes discomfort in the neck or jaw
Less common symptoms
- Sweating
- Pain through from the chest to the back
- Fainting
- Sensations similar to heartburn
When to get help
If you experience angina during physical activity, slow down, stop and use your angina medications. Contact your doctor for a review.
If symptoms do not stop after 15 minutes, treat it as a heart attack and ring for an ambulance (000 in Australia). They will decide whether you should go to hospital.
Atrial Fibrillation
Atrial fibrillation is a very common condition that makes the heart beat irregularly unlike the normal heartbeat that is regular.
The heart normally beats at a regular rate of between 60 and 80 beats per minute.
In atrial fibrillation (also known as AF and A Fib), instead of firing from the sino-atrial node, a number of impulses fire in different areas of upper chambers (atria). This causes individual muscle fibres to contract or fibrillate.
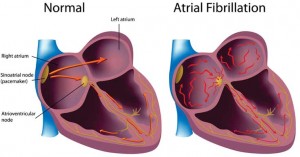
The upper chambers (atria) contract so rapidly that the lower chambers (ventricles) only respond to those impulses that are transmitted to the intermediate node (the atria-ventricular node, between the upper and lower chambers).
Fibrillation of the atria also decreases the amount of time the ventricles have to fill with blood. So the heart does not pump with the same efficiency. This reduces its output (the volume of blood pumped out of the heart to provide oxygen to the body).
Signs and symptoms:
- Irregular heart rate (pulse)
- Dizziness
- Shortness of breath
- Occasionally chest pain
Most people with atrial fibrillation have an underlying heart condition, such as coronary heart disease, heart attack (myocardial infarction), rheumatic heart disease, hypertension (high blood pressure), heart failure, cardiomyopathy, valve disease. It can also be caused by heart surgery.
Cardiac Arrest
Cardiac arrest is the abrupt loss of heart function in a person who may or may not have diagnosed heart disease.
The term “heart attack” is often mistakenly used to describe cardiac arrest. While a heart attack may cause cardiac arrest and sudden death, the terms don’t mean the same thing.
Heart attacks are caused by a blockage that stops blood flow to the heart.
Cardiac arrest is caused when the heart’s electrical system malfunctions. In cardiac arrest death results when the heart suddenly stops working properly. This may be caused by abnormal, or irregular, heart rhythms (called arrhythmias).
A cardiac arrest is an emergency. If you witness a cardiac arrest, you can increase the person’s chances of survival by phoning 000 immediately and giving CPR.
Cardiomyopathy
This covers diseases of the heart muscle. People with these – sometimes called an enlarged heart – have hearts that are abnormally big, thickened, or stiffened. As a result, the heart can’t pump blood as well. Without treatment, these get worse over time. Often, they lead to heart failure and abnormal heart rhythms.
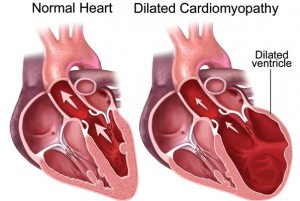
Cardiomyopathy may be genetic, or is caused by high blood pressure, diabetes, obesity, metabolic diseases, or infections.
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
CPVT is a rare inherited heart rhythm disturbance found in young people and children.
Within your heart cells, proteins regulate the release of calcium ions. If these proteins function abnormally, it can lead to a rise in the level of calcium inside your cells. This rise in calcium can cause abnormal heart rhythm.
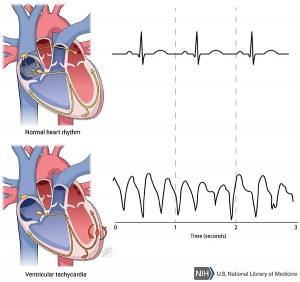
Symptoms
The most common symptoms of CPVT are blackouts, palpitations and dizziness. These can be brought on by strenuous physical activity and heightened emotions, which can cause an increase in the amount of adrenaline running through your blood.
If you experience symptoms, your doctor will refer you to a specialist who will do an exercise test. This is an ECG that records your heart’s electrical rhythm whilst you are exercising. Any abnormal rhythms will show up on the ECG.
Genetic testing can also be done if someone in your family has already been diagnosed with CPVT even if you don’t have symptoms of the condition.
Treatment
Your doctor may prescribe a beta-blocker (a type of medicine) to help slow down your heart rate and help to prevent life-threatening arrhythmias, and restrict the amount of physical activity you do. Roughly 1 in 3 people also need to be fitted with an Implantable Cardioverter Defibrillator (ICD).
Congenital Heart Disease
This is a defect in one or more structures of the heart or blood vessels. It happens before birth.
About eight out of every 1,000 children get it. They may have symptoms at birth, during childhood, and sometimes not until adulthood.
In most cases, scientists don’t know why it happens. Heredity may play a role. Exposure of the fetus during pregnancy to viral infections, alcohol, or drugs may, as well.
Coronary Artery/Heart Disease
You may hear this called CAD. It’s hardening of the arteries that give the heart vital oxygen and nutrients. That hardening can also be referred to as atherosclerosis.
Familial Hypocholesterolaemia
Familial hypercholesterolaemia (FH), is a genetic condition that results in exceptionally high levels of cholesterol in your blood.
If you have Familial Hypercholesterolaemia (FH), your liver can’t remove enough of the bad type of cholesterol (LDL cholesterol) from your blood. This means that the bad type of cholesterol in your blood remains high which can cause a fatty material build up in your arteries which could cause a heart attack.
Heart Attack
Each year, around 54,000 Australians suffer a heart attack. Every 9 minutes someone in Australia has a heart attack.
A heart attack occurs when the narrowing of the artery becomes completely blocked, causing the heart muscle beyond the blockage to become oxygen starved.
Symptoms
The symptoms of a heart attack can be similar to those for angina, with the addition of any or all of the following:
- Dull pain, chest tightness or discomfort that becomes more severe and does not go away
- Jaw and neck pain
- Severe pain that is often described as ‘crushing’
- A squeezing or choking sensation
- Nausea / feeling sick in the stomach
- Fainting
- Sweating
- Pain the shoulder and/or arms
- Pain from the chest to the back
- Similar sensations to heart burn
- Sudden difficulty breathing
- Sudden overwhelming fatigue or weakness
- Flu-like symptoms
If you or someone else experience any combination of these symptoms for more than a few minutes, immediately call 000 for an ambulance.
Heart Failure
The term can be frightening. It doesn’t mean the heart has “failed,” or stopped working. It means the heart doesn’t pump as well as it should. This will cause you to retain salt and water, which will give you swelling and shortness of breath.
Heart Valve Disease
Your valves sit at the exit of each of your four heart chambers. They maintain one-way blood flow through your heart.
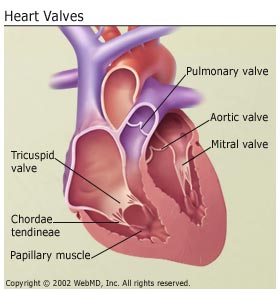
Examples of heart valve problems include:
- Mitral valve prolapse: The valve between your left upper and left lower chambers doesn’t close right.
- Aortic stenosis: Your aortic valve narrows. It affects blood flow from your heart to the rest of your body.
- Mitral valve insufficiency: Your mitral valve doesn’t close tightly enough. This causes blood to leak backwards, leading to fluid backup in the lungs.
Inherited Heart Conditions
Many cardiac disorders can be inherited, including arrhythmias, congenital heart disease, cardiomyopathy, and high blood cholesterol. Coronary artery disease leading to heart attack, stroke, and heart failure can run in families, indicating inherited genetic risk factors.
Genetics can influence the risk for heart disease in many ways. Genes control every aspect of the cardiovascular system, from the strength of the blood vessels to the way cells in the heart communicate. A genetic variation (mutation) in a single gene can affect the likelihood of developing heart disease.
When a family member is diagnosed with heart disease or a heart disorder, other family members are encouraged to undergo screening for risk factors and early stage disease that may not yet produce symptoms.
Share your family history with your healthcare provider to understand your risks.
Pericarditis
A rare condition where the lining surrounding your heart gets inflamed. An infection often causes this.
“https://www.webmd.com/heart-disease/guide/diseases-cardiovascular#1”
“https://www.heartresearch.com.au/heart-disease/heart-conditions/”
